What's New in ARDS
Resolution of ARDS is a multi-faceted process involving various treatment procedures, medications depending on the severity of ARDS and extent of lung damage.
Resolution involves restoring the multiple pathways affected by ARDS, resulting in homeostasis in ARDS.
A 2-pronged strategy involves – a) resolution of inflammation b) restoration of the alveolar–capillary barrier.
Resolution of inflammation – A co-ordinated process that requires the following :
- Neutrophil apoptosis and process to clear excess neutrophils from airspace.
- Alveolar macrophage phenotypes shift from proinflammatory to anti-inflammatory.
- Change of lung lymphocyte populations to T-regulatory cells, orchestrating recovery.
- Chemokine and cytokine balance shifts from proinflammatory to anti-inflammatory.
- The profile of lipid mediators in the airspace transitions from proinflammatory leukotrienes and prostaglandins to proresolving lipid mediators such as lipoxins and resolvins.
Restoration of the alveolar–capillary barrier :
- Lung epithelial growth factors trigger epithelial regeneration through replication and differentiation of resident lung stem-cell populations.
- Restoration of lung epithelial integrity restores alveolar epithelial fluid transport allowing clearance of alveolar oedema.
- Balance of endothelial injury and repair mediators shifts from proinjury angiopoietin-2 dominant to prorepair angiopoietin-1 dominant.
- Restoration of lung endothelial and epithelial glycocalyces.
Pharmacological treatment options like glucocorticoids, surfactants, inhaled nitric oxide, antioxidants, protease inhibitors, and other anti-inflammatory treatments have proven to be ineffective.
One promising therapy includes: - Lung-protective ventilation
Lung-protective ventilation has reduced the mortality of Acute Lung Injury (ALI) from 40% to 25% (from 2000 to 2006). Also, the use of a fluid-conservative strategy for patients with ARDS when they are no longer in shock, has reduced the duration of mechanical ventilation.
It is known that there is no cure for ARDS. All research is done is hence, done to develop strategies and treatment approaches to prevent further damage to the lungs and to medically support the patient while the lungs heal.
Key recommendations :
- Lung protective ventilation (ie, tidal volumes of <6 ml/kg, predicted body weight, and plateau pressure ≤30 mm Hg): Results from a landmark trial (ARMA) shows a reduced mortality and increased days free of ventilation.
- Alternative ventilation strategies have not shown additional benefit compared with lung protective ventilation.
- Airway pressure release ventilation is an innovative pressure-controlled mode of ventilation, delivering prolonged high level of pressure with intermittent, time cycled pressure release to a low level of pressure.
Guideline Recommendations :
- Reserve higher PEEP strategy for patients with moderate-to-severe ARDS.
- What the studies prove:
- Airway pressure release ventilation in acute hypoxaemic respiratory failure suggests a benefit in hospital mortality, ventilation free days, and intensive care unit length of stay (metanalysis, study patient population: 330).
- Higher PEEP without a lung recruitment manoeuvre more beneficial than lower PEEP (mortality benefit was 99%).
- Driving pressure (ie, plateau pressure minus end expiratory pressure) - the key mediator of the benefits of PEEP and tidal volume but may not be useful in predicting mortality because -
- An upper limit of 15 cmH2O for driving pressure is recommended, above which there is considerable lung stress and increased mortality.
- However, couple of clinical trials predicted found increased mortality in the setting of lower driving pressure (ie, ≤15 cm H2O).
- Hence, more research is being carried out.
- Mechanical Power – A novel concept in lung-protective ventilation -
- The amount of energy transferred from a mechanical ventilator to the respiratory system per unit of time is known as mechanical power.
- It is determined by the combined effects of applied tidal volume, driving pressure, respiratory rate, inspiratory flow, and PEEP, as well as determinants of mechanical properties of the lung and may be a better option in lung-protective ventilation as it considers the balance of parameters as a whole.
- Mechanical power can be calculated as:
- Power (J/min)=0·098 × tidal volume × respiratory rate × [PEEP + (0·5 × driving pressure) + (peak pressure–plateau pressure)].
- A study including 8207 patients showed a consistent increase in the risk of death with mechanical power greater than 17 J/min.
- Patients are turned onto their stomachs to improve oxygen levels in the blood.
- In patients with ARDS, it improves oxygenation, increases recruitment potential, and reduces areas of alveolar overdistension ensuring more homogeneous aeration of the lung and potentially reducing ventilator-induced lung injury.
- In a study, prone positioning was associated with an improvement in mortality at day 28 (16% vs 33%, p<0·0001), which persisted at day 90 (24% vs 41%, p<0·0001).
- Prone position in the setting of COVID-19 has been widely implemented and found to be most suitable in the setting of COVID-19 ARDS.
While earlier recommended weakly for the early neuromuscular blockade in patients with moderate-to-severe ARDS, recent trials conducted used these agents in patients with ARDS.
However, the results weren’t very promising as the study itself were halted owing to futility reasons.
- ECMO is a complex procedure where blood is taken out of the body, oxygenated externally, and then returned. It’s high-risk and not suitable for all ARDS patients.
- Two trials have investigated the role of veno-venous ECMO for patients with severe ARDS –
- First trial (CESAR trial) compared the conventional management of ARDS with to an ECMO centre for treatment. An improvement in the quality-adjusted life years was seen at 6 months with patients who were randomised for treatment with ECMO.
- ECMO therapy was delivered in 844 patients, in a trial and an analysis including patients with a PaO2/FiO2 ratio of less than 80 mm Hg indicated ECMO was associated with reduced mortality compared with conventional therapy.
- Overall, patients with severe ARDS (defined as a PaO2/FiO2 ratio of <50 mm Hg for >3 h, a PaO2/FiO2 ratio of <80 mm Hg for >6 h, or severe hypercapnic respiratory failure [ie, a pH of <7·25 with a PaCO2 ≥60 mm Hg for >6 h]) are recommended to be treated with ECMO.E
- ECMO also benefitted the COVID-19 population.
- With potent anti-inflammatory effects, steroids could be of benefit in ARDS, especially in the setting of COVID-19.
- They are the standard of care for patients with COVID-19 ARDS and are investigated for non-COVID ARDS too.
- The DEXA-ARDS trial -
- Study design: High dose (ie, 20 mg once daily for 5 days) dexamethasone followed by a lower dose (ie, 10 mg once daily for 5 days)in patients with moderate-to-severe ARDS.
- Results: Increase in ventilator free days (4.8 days) was seen in the dexamethasone group and a reduced 60-day mortality (21% vs 36%, between-group difference) was also seen.
- A subsequent study (999 patients with non-COVID-19) also found a mortality benefit in favour of corticosteroid use.
- However, an increased risk of late mortality (ie, day 60 and day 180) was found with methylprednisolone in persistent ARDS, thereby proving an association with increased mortality when steroids were initiated beyond day 14 of ARDS onset.
Mesenchymal stromal cells - One novel therapy of interest
These cells, at a nascent stage, is attractive in targeting multiple therapeutic pathways in ARDS and are known to respond to their biological microenvironment while being a part of the heterogeneous treatment effects in different patient phenotypes.
Vasoactive Intestinal Peptide (VIP) formulations :
The underlying hypothesis of VIP is that underlying hypothesis is that VIP defends AT-II cells, prevents cytokine storm, and increases the lung’s oxygen concentration and gas exchange.
In April 2022, the drug was approved by DCG(I) in India for the management of ARDS in severe COVID-19 patients.
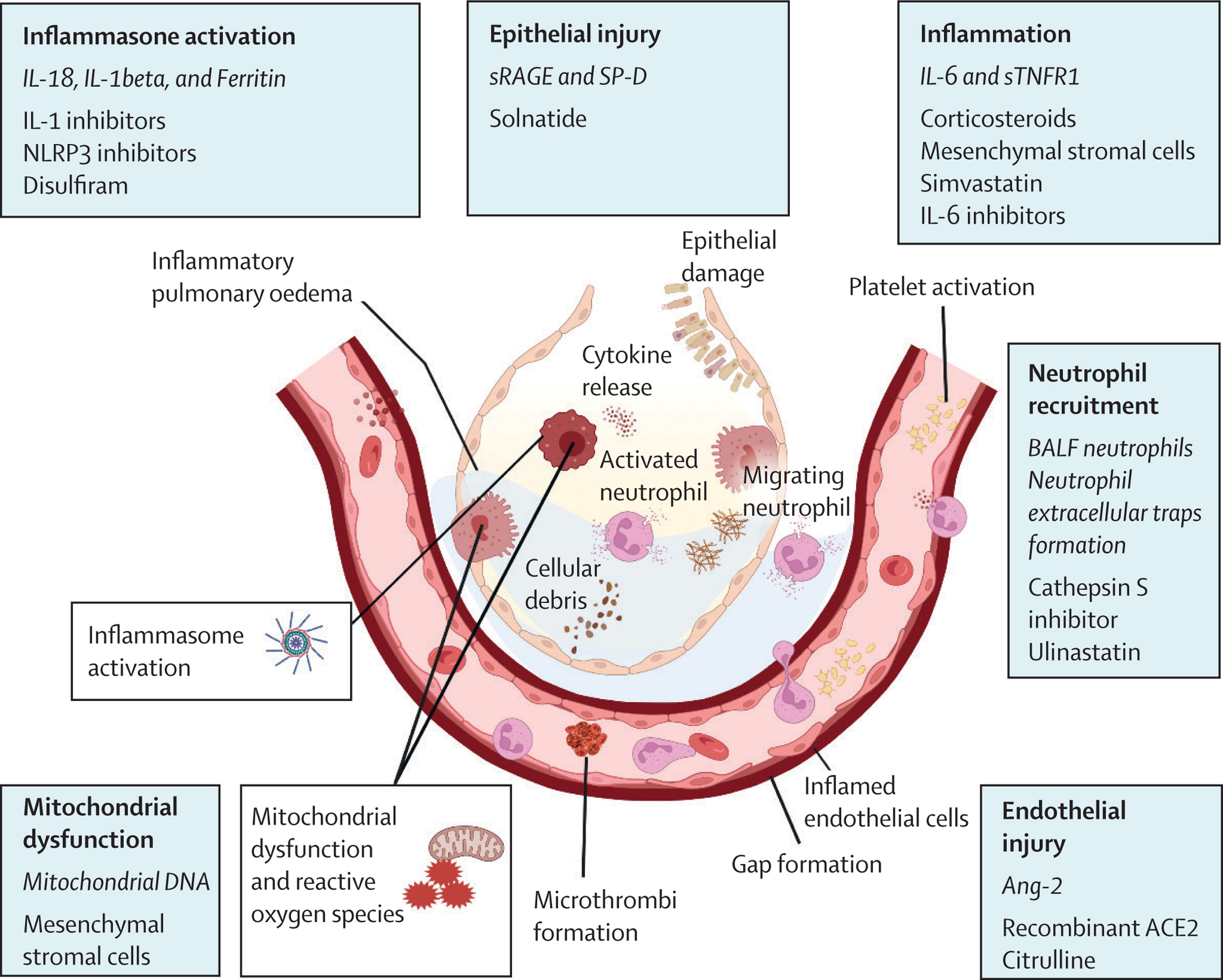
The below figure assesses the various therapeutic targets that could be aligned depending on the pathophysiology of ARDS.
Figure : Potential treatable traits in ARDS, a pathophysiological model.
Aviptadil, a synthetic form of VIP, has been granted a marketing approval in India for the treatment of Acute respiratory distress syndrome (ARDS) in patients with severe COVID-19.
- Vasoactive Intestinal Peptide (VIP) is produced in the body and is highly localized in the lungs. Approximately 70% of it is present in the lungs and some is also present in the nasal mucosa.
- VIP affects the respiratory and immune systems by –
- Relaxing the airway pulmonary vasculature and smooth muscles.
- Inhibits its proliferation.
- Induces bronchodilation and increases pulmonary surfactant production.
- It has an anti-inflammatory effect and defense mechanism against septic shock.
Aviptadil is a synthetic Vasoactive Intestinal Peptide (VIP) that has been studied in respiratory disease conditions like asthma, acute lung injury, pulmonary arterial hypertension, sarcoidosis and idiopathic pulmonary fibrosis and is designated as an ‘Orphan Drug’ by USFDA and EMA. Trials conducted in USA and India shows encouraging results in ARDS associated with COVID-19 patients in terms of reduction in mortality rate and hospital stay.
Evidence showed that the group with ARDS patients treated with Aviptadil survived longer than those who were given the placebo treatment along with the standard of care treatment as recommended by the Government of India. The trial also went on to assess that the patients may experience hospital-free survival rather than ICU survival.
- Oxygenation targets/major treatment guidelines.
- Ventilatory management.
- Adjunctive therapies.
Using respiratory mechanics in ARDS: Calculations and Outcomes.
Respiratory Mechanics during Passive Ventilation
There is a dearth of description for larger groups to understand and interpreting the measured variables of respiratory mechanics – their physiological meanings and reference ranges.
Following charts provide a basis of clinical reference ranges to calculate the Respiratory Mechanics:
| Derived Calculations | Average Value in ARDS* | Estimated Normal Values1 | Explanation of Reference Range |
|---|---|---|---|
| Crs, ml/cm H2O | 38 | 1.6% of VC ml/cm H2O | An average VC in normal subjects is around 4,000 ml; the predicted Crs would be 1.6% X 4,000=64 ml/cm H2O |
| CL, ml/cm H2O | 55 | 2.9% of VC ml/cm H2O | Roughly predicted range: 90-140 ml/cm H2O |
| Ccw, ml/cm H2O | 125 | 3.6% of VC ml/cm H2O | Roughly predicted range: 100-200 ml/cm H2O |
| Ers, cm H2O/L | 26 | 0.62 cm H2O/1% VC (L) | An average VC in normal subjects is 4 L; this gives a predicted Ers as 0.62 / 4% = 16 cm H2O |
| EL, cm H2O/L | 18 | 0.34 cm H2O/1% VC (L) | An average predicted value would be around 9 cm H2O/L |
| Ecw, cm H2O/L | 8 | 0.28 cm H20/1% VC (L) | An average predicted value would be around 7 cm H2O/L |
| EL/Ers | 0.70 | 0.55 | Estimated from predicted values of EL and Ers |
| Rrs, cm H2O/L/s | - | 8-12 at 60 L/min of square- wave inspiratory flow | This reference value is valid for inspiration only and depends on flow rate and the size of endotracheal tube |
Definition of abbreviations : ARDS = acute respiratory distress syndrome; Ccw=chest wall compliance; CL = lung compliance; Crs = respiratory system compliance; Ecw=chest wall elastance; EL-lung elastance; EL/Ers = the ratio of lung elastance to respiratory system elastance; Ers = respiratory system elastance; Rrs = respiratory system resistance at inspiration; VC = vital capacity.
*Mean values reported in or derived from Chiumello and colleagues (83), in which 6 ml/kg Vr and 5 cm H2O of positive end-expiratory pressure were used in 24 patients with moderate or severe ARDS.
*Mean values reported in or derived from D'Angelo and colleagues (65) on 18 anesthetized paralyzed patients for minor surgery in the supine position. Predicted VC for men (L) = 5.76 x height (m)-0.026 X age (yr)-4.34; for women (L)=4.43 × height (m)-0.026 X age (yr)-2.89.
Specific studies and formulas concluded the following findings –
- The use of small Vt, low ΔP, and low Pplat in ARDS is supported by physiological data and controlled trials.
- The use of PEEP to minimize cyclic derecruitment, atelectrauma, inhomogeneity, and stress raisers has a strong biologic rationale.
- Despite the improvements in mortality with the use of these concepts, controversy remains with respect to titration of Vt and PEEP.
- Measurement of ΔP, Pl, or strain allows individualized Vt prescriptions to minimize the risks of VILI.
- Similarly, bedside assessment of recruitment may allow clinicians to determine patients most likely to benefit from the application of a high PEEP.
The following table summarizes and compares four guidelines and their treatment options:
| The Intensive Care Society and the Faculty of Intensive Care Medicine | The French Intensive Care Society | The American Thoracic Society, European Society of Intensive Care Medicine, and the Society of Critical Care Medicine | WHO living guideline (COVID-19 ARDS) | |
|---|---|---|---|---|
| Non-invasive ventilation | - | - | - | Conditional recommendation in mild ARDS |
| Lung protective ventilation | Recommended | Recommended | Recommended | Recommended |
| Prone positioning | Recommended in moderate-to-severe ARDS | Recommended PaO2/FiO2, ratio <150 mm Hg | Recommended in severe ARDS | Recommended PaO2/FiO2, ratio <150 mm Hg |
| Highly positive end expiratory pressure strategy | Recommended in moderate-to-severe ARDS | Recommended in moderate-to-severe ARDS | Recommended in moderate-to-severe ARDS | Conditional recommendation for moderate-to-severe ARDS |
| Driving pressure | - | No recommendation due to insufficient evidence | Research recommendation | Consider driving pressure as part of an individualised positive end expiratory pressure titration strategy |
| Spontaneous ventilation | - | No recommendation due to insufficient evidence | Research recommendation | - |
| Recruitment manoeuvres | - | Not recommended | Not routinely recommended | - |
| High-frequency oscillatory ventilation | Not recommended | Not recommended | Not recommended | - |
| Extracorporeal membrane oxygenation | Recommended in severe ARDS | Recommended when PaO2/FiO2, ratio is <80 mm Hg or lung protective ventilation is not possible | Research recommendation | Conditional recommendation for when PaO2/FiO2, ratio is <80 mm Hg despite lung protective ventilation |
| Extracorporeal carbon dioxide removal | Research recommendation | No recommendation due to insufficient evidence | Research recommendation | - |
| Conservative fluid strategy | Recommended | - | - | Recommended |
| Neuromuscular blockade | Recommended in early moderate to severe ARDS | Recommended in early ARDS with a PaO2/FiO2, ratio of <150 mm Hg | - | Not routinely recommended for all patients |
| Inhaled vasodilators | Not recommended | Can be used when hypoxaemia persists despite lung protective ventilation and prone position and before extracorporeal membrane oxygenation | - | - |
| Corticosteroids | Research recommendation | - | - | Recommended |
| Other pharmacological agents | - | - | - | IL-6 receptor blockers (eg. tocilizumab or sarilumab) or baricitinib (Janus kinase inhibitor) is a strong recommendation. monoclonal antibodies (casirivimab and imdevimab) is a conditional recommendation for patients who are seronegative |
ARDS = Acute Respiratory Distress Syndrome. PaO2 = Partial Pressure of Arterial Oxygen. FiO2 = Fraction of inspired Oxygen.
Table : Guideline recommendations for ARDS management
In ARDS, nutrition support is necessary to prevent cumulative caloric deficits, malnutrition, loss of lean body mass, and deterioration of respiratory muscle strength.
It was also seen that early delivery of enteral nutrition was associated with the modulation of stress and the systemic immune response as well as the attenuation of disease severity.
The American-European Consensus Conference on ARDS recommends :
“Nutritional supplementation should be attempted after a few days of critical illness because of its associations with a more favorable outcome.”
- The administration of nutrition depends on the patient’s underlying illness, with the primary focus falling on the level of gastrointestinal function.
- Conditions such as severe acute pancreatitis, intestinal failure, and sepsis-induced ileus require the use of parenteral nutrition.
- In most cases, Enteral nutrition is the preferred nutritional support method due to its reduced septic risk, lower cost, and role in maintaining the gastrointestinal barrier function.
- Evidence have proven that enteral nutrition may, in fact, be superior to parenteral nutrition in affecting clinical outcomes of ARDS patients.
- Choice of enteral access is decided by the patients aspiration risk. Patients with a known potential for delayed gastric emptying (sepsis, diabetic gastroparesis, head trauma, or narcotic use) are most likely to benefit from post pyloric enteral tube placement since this method would minimize GERD and may result in greater success.
- Energy requirements in ARDS: Energy requirements are different in different cases of ARDS patients. Indirect calorimetry (IC) is the most accurate method for measuring energy expenditure in hospitalized patients. Initial measurements are used at the time of nutritional support’s initiation and may be varied as the energy expenditure changes depending on patients condition.
- High ventilator settings might make using IC unfeasible. An alternative method, reverse Fick equation is used to when oxygen consumption (and, therefore, energy requirements) need to be determined. This happens If an ARDS patient requires hemodynamic monitoring via pulmonary artery catheter.
- Using general calculations, an additional method for determining energy requirements using body weight is promoted by researchers. In this, providing the critically ill patient with 25 to 30 kcal/kg per day has been recommended. These are standard energy requirements.
- Increased protein energy requirements are seen due to rapid protein turnover known to occur in hypermetabolic states with protein requirements ranging from 1.2 to 2 g/kg per day in sepsis and trauma.
- Excessive carbohydrate (exceeding 5 mg/kg per minute) may significantly increase work of breathing in severely stressed patients.
- Nutritional-support regimens that provide a balance of carbohydrate and fat as nonprotein energy should be adequate for optimal substrate utilization. If significant hypercapnia limits successful ventilator management and/or weaning, total energy intake should be evaluated to ensure that adequate (but not excessive) calories are provided. A reduction in carbohydrate intake may be useful if significant hypercapnia persists.
Immunonutrition was an emerging concept applied to ARDS which involves the modulation of the immune system by some dietary nutrients and these supplementary immunonutrients may alter the course of critical illness following sepsis, trauma, or surgery. Special formulas of immunonutrients are available, consisting of a combination of antioxidant vitamins (vitamin C, vitamin E, beta‐carotene), trace elements (selenium, zinc), essential amino acids (glutamine, arginine) or essential fatty acids, such as omega‐3 fatty acids (eicosapentaenoic acid, docosahexaenoic acid), and gamma‐linolenic acid (GLA). In patients with ARDS, significant imbalance in the antioxidant system with a relative increase in oxidative stress leads to increased alveolar injury. And in general, antioxidants supplementation shows a favorable outcome. While recognition of the potentially beneficial role of antioxidants in treating the inflammatory response exists, there are no specific recommendations for supplementation.
What are the other enteral formula options ?
- A reduced-carbohydrate formula supplemented with eicosapentaenoic acid and g-linolenic acid
Eicosapentaenoic acid and g-linolenic acid are precursors of prostaglandins of the 1 and 3 series and leukotrienes of the 5 series and they have anti-inflammatory properties that include vasodilation, inhibition of platelet aggregation, and reduced release of free oxygen radicals while also reducing the arachidonic acid metabolites thromboxane A2 and prostaglandin E2 responsible for the inflammatory cascade and the resulting lung injury of ARDS.
Studies prove that patients receiving a formula supplemented with eicosapentaenoic acid and g-linolenic acid showed significant improvements in oxygenation by the fourth day of the study and reductions in both ventilator time (11 days versus 16.3 days in control group, P=.011) and length of stay in the intensive care unit (12 days versus 17.5 days control group, P=.016). Also, patients receiving the formula had lower number of neutrophils in recovered BAL fluid on the fourth study day and throughout the study period.
Prognosis or healthcare outcomes in ARDS :
Even with emerging therapies, ARDS remains a devastating clinical problem with high rates of morbidity and mortality. Understanding some prognostic factors associated with ARDS may assist in facilitating risk stratification and developing new therapeutic interventions to improve clinical outcomes.
- Clinical predictors for short-term and hospital mortality in ARDS consistent as follows :
- older age, worse physiologic severity of illness (as measured by severity scores such as the Acute Physiology and Chronic Health Evaluation (APACHE) or Simplified Acute Physiology Score (SAPS)), shock on hospital admission, arterial pH less than 7.30, liver disease, early air leak, immunosuppression, triggering risk factor, and right ventricular dysfunction.
- However, after treatment with lower tidal volume ventilation, these remain to be just –
- severity of illness as measured by APACHE II or APACHE III
- age, and
- the presence of non-pulmonary organ failures.
- Effects of race and ethnicity on mortality: A study predicted that African American and Hispanic patients have a higher mortality from ARDS than Caucasian patients and that maybe because of a mutation.
- Diabetes :
- A study showed that diabetes mellitus is not associated with development of ARDS in a large cohort of critically ill patients but might affect the outcomes as patients with diabetes had higher mortality regardless of ARDS status.
- Short-term outcomes vs long-term outcomes :
- Most studies focus on short-term mortality in ARDS but long-term mortality after ARDS and other critical illness is substantially higher than short-term mortality.
- A study showed that patients hospitalized with ARDS (646 patients) showed substantially higher mortality at 1 year compared to in-hospital mortality (41 % vs. 24 %, p < 0.001). The independent predictors of death at 1 year were age, living somewhere other than home prior to admission, and serious comorbidities such as HIV and malignancy.
- Physiological parameters and oxygenation :
- Patients treated with lower tidal volumes with lower mortality as compared to higher tidal volumes with higher mortality had lower inspiratory plateau pressures.
- Also, an elevated ratio of pulmonary dead space (calculated by the mean expired carbon dioxide fraction) to tidal volume (VD /VT) within 24 h of onset of ARDS was associated with higher mortality.
- Oxygenation :
- In short-term ARDS outcomes, the PaO2/FiO2 ratio measured using PEEP ≥ 10 cmH2O and FiO2 ≥ 0.5 at 24 h after ARDS onset showed substantial improvement in risk stratification for short term ARDS mortality.
- Studies showed that, “PaO2/FiO2 with conventional therapy is a prognostic factor of better outcome in patients with ARDS.”
- Genetic polymorphisms :
- A number of genetic polymorphisms have been shown to be associated with mortality in ARDS, in genes including angiotensin-converting enzyme, extracellular superoxide dismutase, duffy antigen/receptor for chemokines, and vascular endothelial growth factor. A variety of biomarkers involved in the pathogenesis of endothelial and epithelial injury, inflammatory response and coagulation have been explored.
A case study on emerging treatment strategies
Patients with respiratory failure COVID-19 in nature were randomized 2:1 to receive 3 days of IV Aviptadil or placebo.
Results were seen as follows :
- Aviptadil showed statistically significant two-fold odds of improved survival at the end of a 60-day period.
- A significant improvement in respiratory distress ratio and reduced interleukin 6 cytokine release was seen by day 3.
- Subjects on mechanical ventilation also experienced 10-fold increased odds of survival with drug versus placebo.
- Aviptadil was also seen to have an acceptable safety profile.
Primary Care for patients
- Post discharge from the ICU, patients with ARDS may have –
- A lower quality of life.
- Significant weakness from neuropathy or myopathy.
- Persistent cognitive impairment.
- Delayed return to work.
- Psychiatric illness is also common after ARDS :
17% to 43% of survivors report depression, 21% to 35% report posttraumatic stress disorder, and 23% to 48% report anxiety. These illnesses may have an increased risk of developing if there is :-
- a longer time to resolution of lung and multiorgan dysfunction, the use of systemic corticosteroids, acquisition of illness in the ICU.
- Many patients report social isolation and sexual dysfunction.
- Some harmful health effects of ARDS may be permanent. The caregiver should be made aware of this along with the patient.
- Although lung function approaches normal at five years, six-minute walking distance, physical function, and quality-of-life measures often remain decreased.
Hence, it is imperative that primary care physicians initiate, coordinate, and monitor continuing services for these patients.
Physicians should assess functional status at hospital follow-up and subsequent visits, ensuring that a multidimensional health care team (e.g., physical and occupational therapists, rehabilitation and home health care nurses, subspecialists) is used to promote optimal health and function.
Primary care physicians should screen for mental health disorders and treat or refer patients as needed.